Dementia Discovery That is Leaving Doctors Speechless (Try This Tonight)
Better than Morphine For Joint Pain… Yet Safer Than Aspirin?
Retire With Freedom. Start Earning Extra Cash Today.
Cervical screening, commonly known as a smear test, is a crucial procedure for women of all ages. However, as women cross the threshold of 50, the importance of this test becomes even more pronounced. This comprehensive guide aims to shed light on the significance, procedure, and frequency of smear tests for women over 50.
Key Takeaways:
- Understanding the importance of pap smear tests for women over 50 and how they can prevent cervical cancer.
- Insights into how often a cervical screening appointment should be conducted for women over 50.
- Practical advice on preparing for pap screening tests and what to expect during the procedure.
The Importance of Smear Tests After 50
As women age, the risk of cervical cancer does not necessarily diminish. In fact, the smear test remains an essential health check for women over 50 just as much as it is for younger women. Cervical cancer screenings detect abnormal cervical cells on the cervix that could potentially develop into cancer. Early detection through a smear test can lead to timely treatment and a significantly better prognosis.
Despite a common misconception, the need for cervical screening does not end as women approach menopause. The Human Papillomavirus (HPV), which is the primary cause of cervical cancer, can be dormant for decades before it causes cell changes.
Therefore, continuing regular smear tests beyond the age of 50 is crucial for ongoing health monitoring.
Frequency of Smear Tests for the Over-50s
The question of “how often smear test over 50” is a common one. Generally, it is recommended that women over 50 continue to have smear tests every five years if previous tests have been normal. This can help with detecting before cervical cancer develops or catching it in its early stages.
This frequency may vary depending on individual health circumstances and the guidelines set by healthcare authorities in different regions.
It’s important to note that even if a woman is no longer sexually active, the smear test remains important. HPV can remain in the body for many years, and changes in the cervix can still occur.
Sticking to the recommended schedule for pap tests is a key component of preventive health care for women in this age group.
Preparing for Your Smear Test
Preparation for a pap test is straightforward. Women are advised to schedule their test for a time when they are not menstruating, as this can affect the results.
It’s also recommended to avoid sexual intercourse, using tampons, or applying any creams or medications to the vaginal area for at least 24 hours before the test.
When scheduling the test, it’s important to inform the healthcare provider if you have any special needs or if you’re experiencing symptoms such as unusual vaginal bleeding or pain. This information can help the provider ensure that the test is as comfortable and effective as possible.
What Happens During the Test?
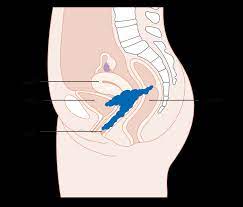
The smear test is a quick and simple procedure. During the test, a healthcare professional will gently insert a speculum into the vagina to hold it open.
Then, they will use a small brush or spatula to collect cells from the cervix. While the test can be uncomfortable for some, it should not be painful.
After the sample is collected, it is sent to a laboratory for analysis. If the results show abnormal cells, further testing may be necessary. It’s important to remember that abnormal results do not always indicate cancer; they can also be due to other less serious conditions.
Understanding Your Smear Test Results
Once the cervical cancer screening test is completed, the waiting period for results can be a source of anxiety for many women. However, understanding what the results mean can help alleviate some of this stress.
A normal result means that no abnormal cells were found, and you can continue with the regular screening schedule.
If the results are abnormal, it does not necessarily mean you have cervical cancer. It indicates that cell changes have been detected, and further investigation is needed.
Your healthcare provider will guide you through the next steps, which may include a repeat smear test or a more detailed examination called a colposcopy.
The Role of HPV Vaccination
The HPV vaccine has significantly impacted the prevention of cervical cancer, and it’s not just for the younger population. Women over 50 who have not been vaccinated can still benefit from the vaccine. While it cannot treat existing HPV infections, it can prevent new infections by other HPV strains.
Discussing the option of HPV vaccination with your healthcare provider is a proactive step in cervical cancer prevention. The vaccine, in conjunction with regular smear tests, or an HPV test offers a comprehensive approach to maintaining cervical health.
Addressing Common Concerns and Misconceptions
Many women over 50 have concerns about the smear test, ranging from discomfort during the procedure to the fear of receiving bad news. It’s important to address these concerns with your healthcare provider, who can provide reassurance and information.
There are also misconceptions that smear tests are not necessary after a certain age or after menopause. However, as long as a woman has a cervix, regardless of her age or sexual activity, smear tests remain an important health check.
Clearing up these misconceptions can encourage more women to attend their regular screenings.
The Future of Cervical Screening
Cervical screening is evolving, with new technologies and methods being developed to improve accuracy and comfort.
For example, HPV tests are becoming more common as a primary screening tool, which may change how often smear tests are recommended.
Staying informed about the latest developments in cervical screening can help women make educated decisions about their health. As research continues, the goal is to make cervical cancer a preventable disease for all women, regardless of age.
Summary
Smear tests for women over 50 are a critical component of preventive healthcare. Regular screening can detect cervical changes early, leading to timely treatment and a better chance of a positive outcome.
Women in this age group should adhere to the recommended frequency of every five years for smear tests unless advised otherwise by their healthcare provider.
Preparation for the test is minimal, and while the procedure may cause some discomfort, it is usually quick and straightforward. Understanding the results and the role of HPV vaccination can empower women to take charge of their cervical health.
Addressing common concerns and staying updated on screening advancements are also key to ensuring that women over 50 continue to prioritize this important test.
FAQ Section
Q: How often should women over 50 have a smear test? A: Women over 50 should have a smear test every five years if their last cervical screening was normal. This frequency may be adjusted based on individual risk factors such as family history, medical history, and regional healthcare guidelines.
Q: Is a smear test necessary for women who are no longer sexually active? A: Yes, a smear test is still necessary for women who are no longer sexually active. HPV can remain in the body for many years, and cervical changes can occur regardless of current sexual activity.
Q: What should I do if my smear test results are abnormal? A: If you have an abnormal pap test, it’s important not to panic. Abnormal results often indicate cell changes that require further investigation but do not necessarily mean you have cancer. Your ob-gyn doctor will guide you through the next steps, which may include additional testing or a colposcopy.
Disclaimer: The information in this article is intended for educational and entertainment purposes only and should not be used instead of or contrary to that of a medical professional. Before taking supplements, starting a new diet, or embarking on a new exercise regime please consult a medical or nutritional professional. The owners of “Getting Healthy After 50” are not medical professionals and are simply redistributing information that is freely available on the internet.