Dementia Discovery That is Leaving Doctors Speechless (Try This Tonight)
Better than Morphine For Joint Pain… Yet Safer Than Aspirin?
Retire With Freedom. Start Earning Extra Cash Today.
Coronary Artery Spasms Causes – What You Should Know
A coronary artery spasm is a temporary sudden contraction of the wall of one of the arteries that supply blood to the heart (coronary). This obstruction usually lasts from seconds to minutes and can cause severe chest pain.
The cause is not known. It may be caused by plaque in an artery rupturing or causing a clot that blocks blood flow to the heart muscle. Other potential triggers include infection, cocaine use, and preeclampsia (a condition related to pregnancy). In some cases, no cause is found.
The pain caused by a coronary artery spasm is usually not due to a heart attack (myocardial infarction) or angina (a type of chest pain). It may be mistaken for these conditions.
Common triggers include:
In addition, other causes are postulated including:
Drugs that can cause coronary artery spasm include ephedrine, cocaine, and amphetamines. These drugs induce catecholamine release from the adrenal gland and medulla in high concentration. An increased concentration of catecholamines in the blood can stimulate alpha-1 receptors on endothelial cells and smooth muscle cells which are present in large quantities in the arterial wall. The rise in the concentrations of catecholamines also causes calcium to leave the cells which are normally buffered by it.
This results in a sudden spasm of the valves and muscular walls, which in turn squeezes the blood out of the vessel, resulting in pain and heat sensations to the area adjacent to the site of obstruction.
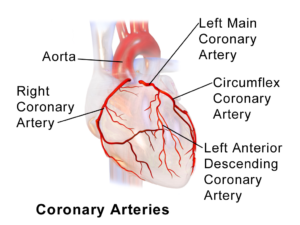
If a coronary artery spasm is not treated properly it may become more severe. If further deterioration is not prevented there may be no other choice than emergency revascularization with percutaneous transluminal coronary angioplasty (PTCA) or laser angioplasty (LASER). Incomplete flow through the coronary artery may result in ischemic heart disease (IHD) and eventually fatal angina.
A coronary artery spasm may be treated with nitroglycerin (NTG), which is a vasodilator. An initial dose of NTG may be given to relieve the pain. The dose must be repeated every 10–15 minutes if necessary until symptoms have disappeared. Other medications that are used are papaverine, glyceryl trinitrate, or calcium channel blockers.
Another method of treatment is to administer a drug called an anticoagulant. This will prevent the formation of blood clots. Examples include heparin or vitamin K antagonists, which are sometimes used together with an anticoagulant. This is not as effective as PTCA or LASER but does not have any significant adverse effects, and may be less expensive than other treatments.
Coronary spasms are dangerous because they can cause heart attacks if symptoms become serious enough (ischemic heart disease). However, the mortality rate for a coronary artery spasm is relatively low compared to other causes of unstable angina; up to 19% in otherwise healthy people, according to some studies. The mortality rate is higher in women and the elderly.
Men have a much higher incidence than women. The average age of onset is around 60 years with a peak frequency between 65 and 75 years. It is rare in children, which might be explained as coronary artery spasms requiring some degree of atherosclerotic changes, which usually preexist since childhood in the over 65-year-old cohort.
A coronary artery spasm may result in a heart attack (myocardial infarction) if the spasm causes complete blockage of an artery or triggers an unstable plaque that suddenly ruptures.
The mortality rate is low when the spasm is mild. It is thought that a small amount of plaque may be squeezed into the coronary artery, causing a mild spasm. This can then lead to a heart attack if the spasm becomes larger. However, only 40% of these cases result in a heart attack and only 15% result in death, indicating that the majority of people who suffer from coronary spasms are not killed by them.
Coronary artery spasms may trigger an unstable plaque to suddenly rupture or produce another complication such as an embolus (blood clot) that causes heart blockage (cardiac arrest) or atrial fibrillation (irregular tachycardia).
The first description of coronary artery spasm was in 1891 by Ernst S. Bailey who described the pain as “characteristic” and referred to the “asthma-like” attack. In 1908, F.C. Moore and G.W. Beecher noted that the pain was pleuritic indicating a possible origin in the pleura, which is confirmed by later studies such as Sando’s 1968 report which found that visualization of inflamed fat cells in the pulmonary artery during a coronary artery spasm strongly suggests its origin there.
Some additional information can be gathered from The American Heart Association website and from their Fact Sheets.
GeneSigDB A database of single-gene diseases with cardiovascular manifestations.
Disclaimer: The information in this article is intended for educational and entertainment purposes only and should not be used instead of or contrary to that of a medical professional. Before taking supplements, starting a new diet, or embarking on a new exercise regime please consult a medical or nutritional professional. The owners of “Getting Healthy After 50” are not medical professionals and are simply redistributing information that is freely available on the internet.